Catheterization | Hong Kong Asia Heart Centre
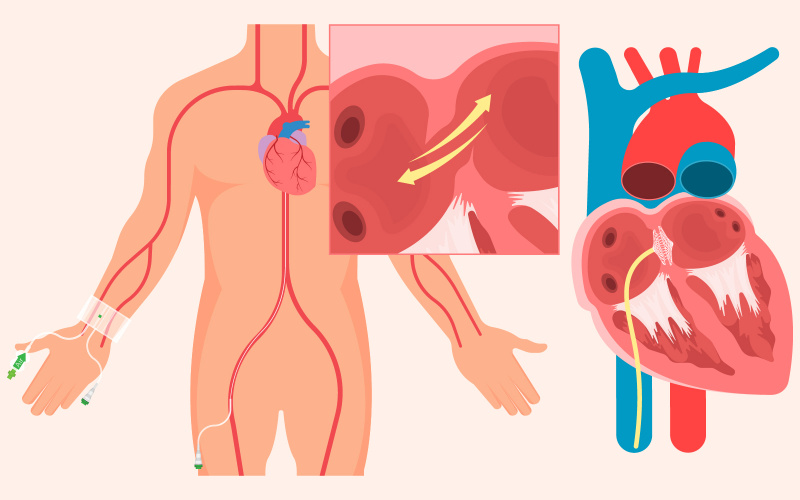
Cardiac Catheterization And Percutaneous Coronary Intervention (PCI)
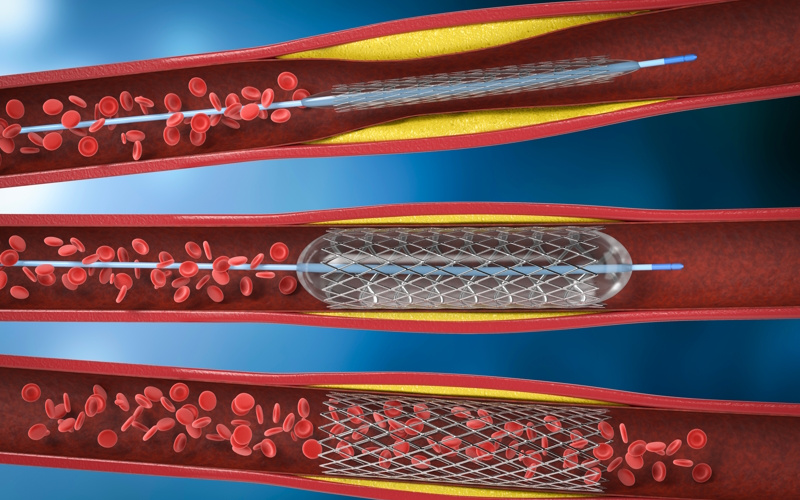
Cardiac catheterization is used to investigate the structure and function of the heart. Coronary Angiogram is used to investigate for any narrowing of the coronary arteries (arteries that supply blood to heart muscle). When indicated, percutaneous coronary intervention (PCI) can be performed at the same setting of cardiac catheterization and coronary angiogram.Cardiac catheterization can provide in-depth and specific information of various cardiac diseases. Coronary angiogram can provide a clear picture of the severity of narrowing of coronary arteries. In general, both are superior to non-invasive procedures and can help doctor make a definite plan of management. In emergency situation caused by acute coronary syndrome (heart attack), the procedure is essential in diagnosis. It is also a stepping stone to coronary intervention, which serves to open up the artery and improve the heart function. This approach, despite its high risk, can be life saving and the consequence can be detrimental if it is delayed.Proccess (Intervention Demo Video):This is an invasive procedure that is generally performed under local anesthesia in the Cardiac Catheterization & Intervention Laboratory (CCIL).Electrodes are adhered to the chest to monitor the heart rate and rhythm. Blood oxygen monitor through your fingertip will be set up. Measurement of blood pressure from your arm will be taken during the examination.A small wound is made either from the wrist or the groin for access to arteries or veins. Catheters are advanced to the heart under X-ray guidance.Pressures within the heart are measured.Contrast is injected and films are taken. Narrowing of the coronary arteries is identified.In general, a special catheter is placed in a coronary artery with narrowing. A guide wire is passed through the narrowing. The guide wire is used as a track to allow a balloon to go to the narrowing. The balloon is inflated to open up the artery. A stent is then deployed permanently inside the artery to keep it patent.Type of Stent : Bare Metal Stent, Drug Eluting Stent(DES), Bio-Resorbable Stent, Partly Resorbable Stent (Bioadaptor)During the procedure, you will be asked to hold your breath or cough. Transient chest pain may be experienced during balloon dilatation. If you experience severe or persistent chest pain, dizzy spell or any discomfort, you are required to inform the staff.Other techniques may be adopted to improve the success and outcome of the procedures. Please discuss with your doctor the procedure involved as new advance in PCI cannot be fully discussed in this information sheet.After Surgery:Usually you can be discharged 1 day after the procedure.The wound will be inspected and covered with light dressing. Please keep the wound site clean and change dressing if wet. In general, showers are allowed after 2 days.Please avoid vigorous activities (household or exercise) in the first 7 days after the procedure.Bruising around the wound site is common and usually subsides 2-3 weeks later. If you notice any signs of infection, increase in swelling or pain over the wound, please come back to the hospital or visit a nearby Accident and Emergency Department immediately.
Left Atrial Appendage Occlusion (LAAO)
Atrial fibrillation is the most common
heart rhythm disturbance. There are seventy thousand people with AF in the HK.Atrial fibrillation makes your risk of a
stroke five times higher.When your heart beats normally, its muscle
walls squeeze (contract) to force blood out of the heart and around the body.If you have atrial fibrillation, your
heartbeat is irregular and fast, your heart may not have a chance to empty
properly before filling up with blood again. Blood can collect inside the upper
chamber of the left side of the heart, and this increases the risk of blood
clots forming.If blood clots form in your heart, there is
a risk they can travel in your bloodstream towards your brain. If a clot blocks
one of the arteries leading to your brain, it could cause a stroke. About 90%
of the blood clots that cause stroke are also formed in the left atrial
appendage(LAA). Stroke prevention is the most important part of atrial
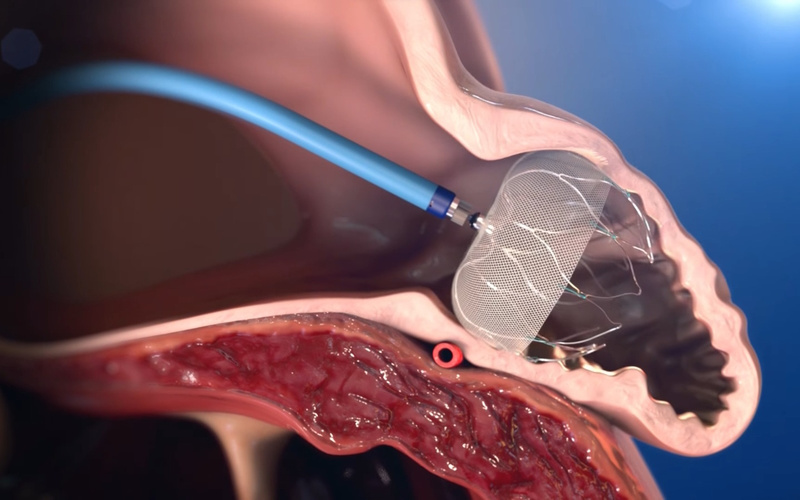
fibrillation treatment.Promotion VideoProccess:During the process, the patient needs
general anesthesia or monitoring anesthesia, which is done in the cardiac
catheterization laboratory with the help of transesophageal ultrasound and
X-ray fluoroscopy. The cardiologist will insert a catheter into the femoral
vein on the inner thigh of the patient, and implant the occluder into the left
atrial appendage through atrial septal puncture. The occluder is like a
parachute blocking the entrance of the left atrial appendage. After the
parachute opens, it will interact with the heart muscle Connected, like a
natural barrier, to prevent the blood from staying in the clot. After the
operation is completed, the patient can get out of bed on the same day. Normally,
the patient will be hospitalized for about 2 to 3 days.After Procedure:Like other surgeries or treatments, LAA
closure surgery also has risks. The doctor will compare the risks of left
atrial appendage occlusion and other appropriate treatments with the patient.During this period, please continue to take
anticoagulant or antiplatelet drugs according to the doctor’s instructions.Swimming is not allowed within one week
after discharge. Use shower as much as possible for bathing, and keep the wound
area clean and dry; avoid lifting heavy objects and avoid excessive strenuous
activities within one week.
Atrial Fibrillation (AF) Pulsed Field Ablation (PFA)
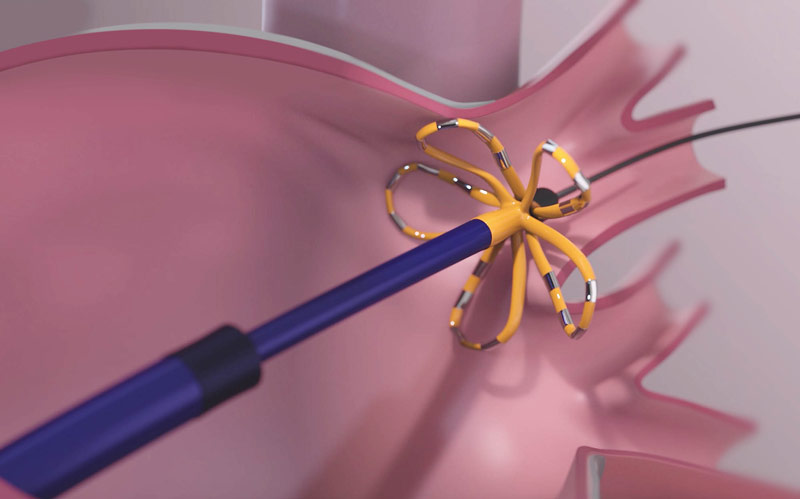
Atrial fibrillation is a common heart rhythm disorder in which patients typically experience an irregular, extremely fast heart rhythm. Here there are the three types:Paroxysmal: last for not more than 7 days, usually within 24 hoursPersistent: last for longer than 7 daysPermanent: last for more than a yearIt is estimated that about 1% of the people in Hong Kong suffer from atrial fibrillation. Based on the current population of about 7 million, that is, more than 70,000 people. Atrial fibrillation may not lead to immediate death, but it is an important chronic disease and leading to severe complications:‧5 times higher in risk of stroke‧3 times higher in risk of heart failure‧About 70% higher in risk of heart attack‧About 40% higher in risk of dementia‧About 4 times higher in risk of deathPulsed field ablation releases a series of high-amplitude electrical field lasting for several microseconds to the target tissue.Strong electric field will make irreparable electrical pores in cell membrane, and the contents of the cell will flow out slowly, finally the cell is destroyed.Pulsed Field Ablation has been approved by the U.S. Food and Drug Administration (FDA) and can be used in patients with persistent or permanent atrial fibrillation. Our center is the first private hospital in Hong Kong to introduce this technology. As the instrument was available in February 2023 , it has been officially put into service.Compared with other ablation techniques, pulse field ablation is easier to operate, and it only takes about 3 minutes to complete the isolation of a pulmonary vein, so the procedure time is shorter and use of anesthetic medication can be minimized.Promotion VideoProccess:This invasive procedure is generally performed in the Cardiac Catheterization & Intervention Laboratory (CCIL). You may undergo general Anesthesia (GA) or Monitored Anesthesia Care (MAC).Electrodes are adhered to the chest to monitor the heart rate and rhythm. Blood oxygen monitor through your fingertip will be set up. Measurement of blood pressure from your arm will be taken during the examination.Small wounds are made over the groin for access to veins.Electrical Field energy will be delivered to the target site as ablation to destory abnormal cells.The duration of the procedure could last around 3 hours.You will be sent to the ward for observation for another 12-24 hours.After Procedure:Usually you can be discharged 1 day after the procedure.The wound will be inspected and covered with light dressing. Please keep the wound site clean and change dressing if wet. In general, showers are allowed after 2 days.Please avoid vigorous activities (household or exercise) in the first 7 days after the procedure.Bruising around the wound site is common and usually subsides 2-3 weeks later. If you notice any signs of bleeding, infection, increase in swelling or pain over the wound, please come back to the hospital or visit a nearby Accident and Emergency Department immediately.During subsequent follow-up, our medical staff will explain to you the results of the procedure and discuss on any subsequent plan of management. You are advised to ask your close relatives to join the interview.
Electro-Physiology Study (EPS) & Radio Frequency Ablation (RFA)
Heart rhythm is mainly controlled by the conduction system of the heart. Any abnormality in the conduction system may result in abnormal heart rhythm (arrhythmia).Electro-Physiology Study (EPS) is a test to find out the cause of arrhythmia. A patient suffering from arrhythmia may have palpitation, chest discomfort, dizziness or vertigo. In severe condition, the patient may lose consciousness or have sudden death. Radio frequency (RF) energy has been used since 1990 to ablate cardiac arrhythmia. This energy is released at the tip of the catheter to local cardiac tissue, within which the conduction property will be lost. The result will be the successful cure of the arrhythmia.Proccess:This invasive procedure is generally performed under local anesthesia in the Cardiac Catheterization & Intervention Laboratory (CCIL). You are alert during the procedure, but we may give you sedation if needed.Electrodes are adhered to the chest to monitor the heart rate and rhythm. Blood oxygen monitor through your fingertip will be set up. Measurement of blood pressure from your arm will be taken during the examination.Small wounds are made over the groin, under the clavicle or around the neck for access to arteries or veins.Catheters are advanced to the heart under X-ray guidance. At specific sites inside the heart, we will record electric information; we then deliver tiny electric current to alter your heart rate and try to trigger arrhythmias.You may experience discomfort when your heart is being excited to certain rate; when an induced arrhythmia is persistent, we may use direct current (DC) cardioversion to convert it.RF energy will be delivered to the target site for around 60 seconds via special RF catheter. You may experience slight chest discomfort during delivery of energy.After RFA, another EPS will be carried out to confirm the success of the procedure.The duration of the procedure could last from 3 hours to over 5 hours depending on the nature and complexity of the arrhythmia.You will be sent to the ward for observation for another 12-24 hours.After Procedure:Usually you can be discharged 1 day after the procedure.The wound will be inspected and covered with light dressing. Please keep the wound site clean and change dressing if wet. In general, showers are allowed after 2 days.Please avoid vigorous activities (household or exercise) in the first 3 days after the procedure.Bruising around the wound site is common and usually subsides 2-3 weeks later. If you notice any signs of infection, increase in swelling or pain over the wound, please come back to the hospital or visit a nearby Accident and Emergency Department immediately.During subsequent follow-up, our medical staff will explain to you the results of the procedure and discuss on any subsequent plan of management. You are advised to ask your close relatives to join the interview.
Mitraclip Surgery
Mitral regurgitation (or “MR”) is a
condition affecting one of the valves in your heart, the mitral valve. The
valves in your heart control the flow of blood through the four chambers of
your heart. Each heart valve is made up of thin, but strong flaps of tissue. As
blood flows through the four chambers of the heart, the valves open and close
to ensure that blood flows in the right direction.
The mitral valve is located between your
heart’s two left chambers and allows blood to flow forward through your heart
during a normal heart- beat. When the mitral valve fails to close completely,
blood flows backward in the opposite direction. This backward flow is called
mitral regurgitation.
Cause:There are several causes of mitral
regurgitation. These include:Heart disease (such as heart failure), or other conditions that causing heart valve annulus dilatationDeterioration of heart tissue leading to valve prolapseCongenital heart valve abnormalities` (abnormal at birth)Rheumatic Heart DiseaseDegenerative change due to aging
Symptom:
In order to compensate the effect of mitral / tricuspid regurgitation, the ventricles would increase its pumping action to maintain enough blood supply to our body. Heart muscle would then be overloaded and becomes enlarged in size and weak. This extra burden on the heart and lungs may lead to heart failure in the long run. There would be insufficient blood supply for the body requirement, and may eventually lead to arrhythmia (irregular heartbeat), stroke, and even sudden death.
Patients with mitral / tricuspid regurgitation might not experience symptoms, or some may have:Tiredness and weaknessShortness of breath (dyspnea), especially on exertion (vigorous movement) or while lying downCough (especially at night or when lying down)Lower Limb edema (swelling)Poor appetiteArrhythmiaPalpitation (feeling of rapid heartbeat)
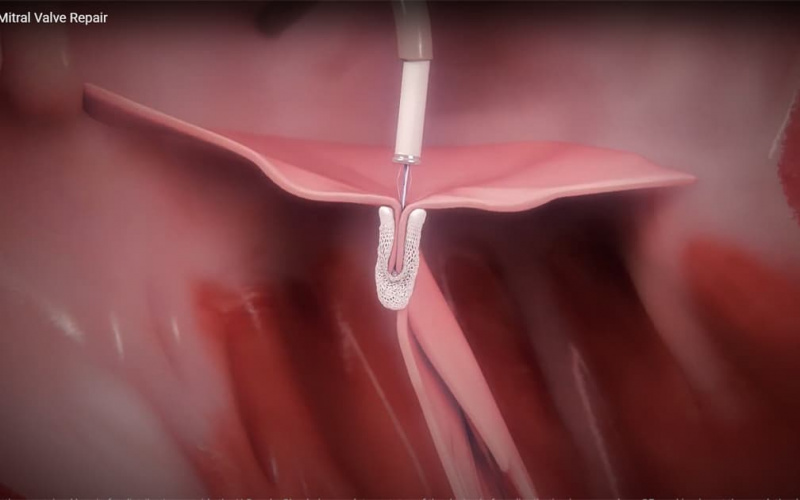
The MitraClip procedure:
A MitraClip procedure is carried out under
a general anaesthesia in catheterization laboratory with assistance of
trans-esophageal echocardiography (TEE) and X-rays. During the procedure,
doctors access the mitral valve with a thin tube (called a catheter) that is
guided through a vein in patient’s leg to reach the heart. The MitraClip is
then clipped to the mitral valve and help it close completely. A procedure
usually takes three to four hours on average but it can vary due to different
anatomies. The length of hospital stay is around one to five days following the
procedure.
MitraClip surgery risks and postoperative
instructions:
The MitraClip is approved by the U.S. Food
and Drug Administration (FDA) and has been used with more than 80,000 patients
worldwide.Your doctor will discuss how the risks of
MitraClip therapy compare with other options that may be available to you.The length of hospital stay is around one
to five days following the procedure.The MitraClip device is very small–less
than the size of a typical fingertip. You will not be able to feel its
presence.Your doctor may also prescribe a blood
thinner after you have received the treatment. It is very important to
carefully follow your doctor’s instructions regarding any medicines you need to
take.Most patients who undergo MitraClip therapy
do not need special assistance at home after the procedure, outside of ongoing
needs for any unrelated health conditions.
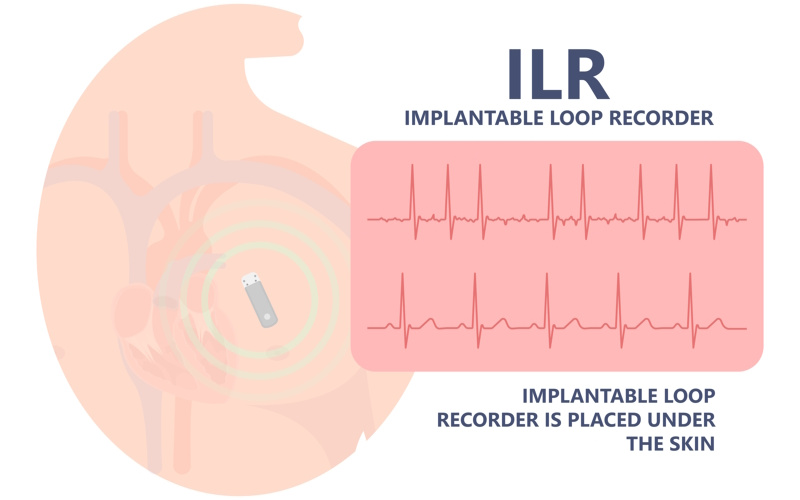
Implantable Loop Recorder (ILR)
Patients may have unexplained recurrent
symptoms of dizziness, palpitation or loss of consciousness. There are many
causes, such as arrhythmias (abnormal heart rhythm). Sometimes, a definitive
diagnosis cannot be made after conventional investigations.
Implantable loop recorder (ILR) is used to
check whether the symptoms are due to arrhythmias. It is a small device
implanted usually under the skin of the left chest wall. It consists of 2
internal electrodes, through which the heart rhythm can be monitored. The
battery can last for >12 months.
Proccess:
This invasive procedure is performed under
local anesthesia in the Cardiac Catheterization & Intervention Laboratory
(CCIL). You are alert during the procedure, but we may give you sedation to
calm you down.A small incision (about 2 cm long) is made
over the left chest wall.The ILR is inserted through the incision
into the pocket underneath the skin.The wound will be closed with suturing
material and covered with dressing.The procedure usually takes about 20-30
minutes.
After Procedure:
You may be discharged from hospital on the
day or 1 day after the ILR implantation.The wound should be covered with light
dressing. Please keep the wound site clean and avoid making the dressing wet
during a bath. Always change dressing if wet.You may need to come back to the centre for
suture removal 1 week after the procedure. You may remove the dressing 2-3 days
after suture removal.Follow your doctor’s instructions or refer
to the information booklet from the ILR company to minimize the risk of
electromagnetic interference. In general, strong electro-magnetic field or
radiofrequency signal will interfere your ILR. Please keep a distance of >15
cm (6 inches) from an active mobile phone. Household electrical or electronic
appliance usually does not affect ILR.Depending on the type of ILR used, you may
be given a hand-held activator for recording of events. We will explain to you
how to operate.When a cause is found using the device, we
may remove the ILR and give you the appropriate treatment accordingly.When battery is depleted, it can be removed
or replaced as decided by your doctor.
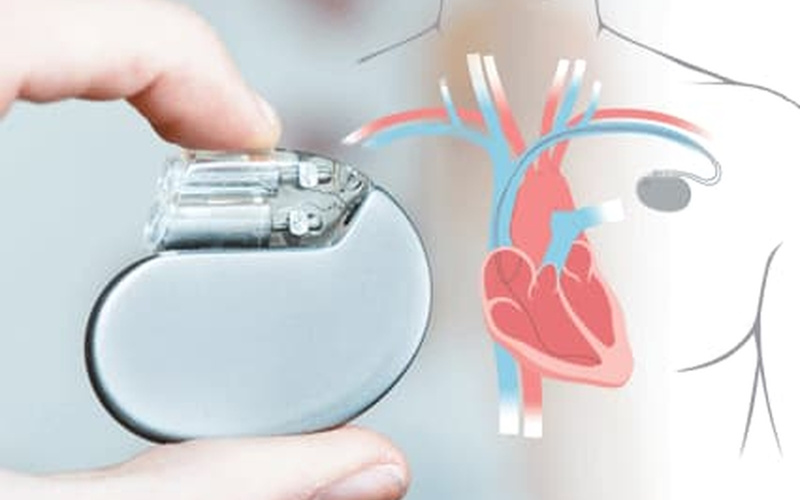
Permanent Pacemaker (PPM)
Heart rhythm is mainly controlled by the
conduction system of the heart. Any abnormality in the conduction system may
result in abnormal heart rhythm (arrhythmia). Arrhythmias with slow heart rate
cause dizziness, syncope, heart failure or occasionally cardiac death.
Permanent cardiac pacemaker (PPM) is an
implantable device used for long-term treatment of arrhythmias with slow heart
rate. It consists of a battery-powered generator and leads which connect the
generator to the patient’s heart. If the heart rate is slow, the pacemaker will
stimulate the heart at a desirable rate.
Proccess:
This invasive procedure is performed under
local anesthesia in the Cardiac Catheterization & Intervention Laboratory
(CCIL). You are alert during the procedure, but we may give you sedation to
calm you down.Electrodes are adhered to the chest to
monitor the heart rate and rhythm. Blood oxygen monitor through your fingertip
will be set up. Measurement of blood pressure from your arm will be taken
during the examination.Skin disinfection will be performed and a
small skin incision (about 3-5 cm long) will be made under your left (sometimes
right) clavicle.Contrast may be injected intravenously to
visualize the veins in your arm and needle puncture under the clavicle may be
required to obtain an access to your vein.1 to 2 leads will be advanced to your heart
chambers through your vein under X-ray guidance.The generator will be connected with the
lead(s) and implanted in a pocket created under the skin or muscle.The wound will be closed with suturing
material and may covered with pressure dressing.The procedure usually takes around 2 to 3
hours.
After Procedure:
You may be discharged from hospital 1-2
days after the PPM implantation.The wound will be inspected and covered
with light dressing. Please keep the wound site clean and change dressing if
wet. In general, showers are allowed after 7 days.You may need to come back to the centre for
suture removal 1 week after the procedure. You may remove the dressing 2-3 days
after suture removal.Please avoid lifting the affected arm for 4
weeks and avoid vigorous arm movement in the first month after the procedure.You will be arranged to attend regular
pacemaker analysis, re-programming and battery power assessment.Please carry your pacemaker identity card
at all times.Follow your doctor’s instructions or refer
to the information booklet from the pacemaker company to minimize the risk of
pacemaker malfunction due to electromagnetic interference. In general, strong
electro-magnetic field or radiofrequency signal will interfere your pacemaker.
Please keep a distance of >15 cm (6 inches) from an active mobile phone.
Household electrical or electronic appliance usually does not affect pacemaker.The generator will need to be replaced in
5-10 years’ time when the battery is depleted.
Cardiac Resynchronization Therapy (CRT)
Heart failure patients have symptoms of
shortness of breath and body swelling caused by decreased pumping of blood from
the heart. Initial management includes treating underlying cause, adopting a
healthy lifestyle and taking medications.
Patients with persistent symptoms despite
the above treatments may consider echocardiography. It is essentially an
implantable cardiac pacemaker that consists of a battery-powered generator and
leads which connect the generator to the patient’s heart. But there is a
special lead placed in the left heart, so that the device can stimulate both
the left and right heart in a coordinated (synchronized) manner. The synchronized
contraction will increase pumping of blood from the heart. Recent studies have
shown that in selected groups of patients, CRT improves heart failure symptoms,
quality of life, exercise capacity and heart function.
Proccess:
This invasive procedure is usually
performed under local anesthesia in a Cardiac Catheterization &
Intervention Laboratory(CCIL). You are alert during the procedure, but we may
give you sedation to calm you down.Electrodes are adhered to the chest to
monitor the heart rate and rhythm. Blood oxygen monitor through your fingertip
will be set up. Measurement of blood pressure from your arm will be taken
during the examination.Skin disinfection will be performed and a
small skin incision(about 3-5cm long) will be made under your left(sometimes
right) clavicle.Contrast may be injected intravenously to
visualize the veins in your arm and needle puncture under the clavicle may be
required to obtain access to your vein.3 leads will be advanced to your heart
chambers through your vein under X-ray guidance. One lead is placed in the
right atrium and one in the right ventricle. A special lead is implanted in a
vein called the coronary sinus that lies on the surface of the left ventricle.
Contrast injection is required to show this vein.The generator will be connected with the
lead(s) and implanted in a pocket created under the skin or muscle.The wound will be closed with suturing
material and covered with pressure dressing.The procedure usually takes around 3-4
hours.
AfterProcedure:
You may be discharged from hospital several
days after the CRT implantation.The wound should be covered with light
dressing. Please keep the wound site clean and avoid making the dressing wet
during shower. Always change dressing if wet.You may need to come back to the ward or
clinic for suture removal 1 week after the procedure if any. You may remove the
dressing 2-3 days after suture removal.Please avoid lifting the affected arm for 1
month and avoid vigorous arm movement in the first week after the procedure.You will be arranged to attend regular CRT
analysis, re-programming and battery power assessment. To maximize the benefits
of CRT, the settings will be optimized with the help of echocardiogram.Please carry your CRT identity card at all
times.Follow your doctor’s instructions or refer
to the information booklet from the CRT Company to minimize the risk of CRT
malfunction due to electromagnetic interference. In general, strong
electro-magnetic field or radiofrequency signal will interfere your pacemaker. Please
keep a distance of >15cm(6 inches) from an active mobile phone. Household
electrical or electronic appliance usually does not affect pacemaker.CRT generator will need to be replaced in
5-10 years’ time when the battery is depleted.
Implantable Cardioverter Defibrillator (ICD)
Heart rhythm is mainly controlled by the
conduction system of the heart. Any abnormality in the conduction system may
result in abnormal heart rhythm (arrhythmia). Life-threatening arrhythmias such
as ventricular tachycardia (VT) and ventricular fibrillation (VF) cause not
only palpitations, dizziness and syncope but also sudden death.
Implantable Cardioverter Defibrillator
(ICD) is an implantable device used for treatment of VT and VF. It is
essentially an implantable cardiac pacemaker which consists of a
battery-powered generator and leads that connect the generator to the patient’s
heart. The lead placed in the right heart has defibrillation function. As soon
as a VT or VF is detected, the ICD will automatically try to correct it by
anti-tachycardia pacing, cardioversion or defibrillation. It has been proven in
various clinical trials that ICD is better than the best anti-arrhythmic drugs
in prolonging survival among patients with a high risk of sudden cardiac death
due to VT or VF.
Proccess:
You may be discharged from hospital a few
days after the ICD implantation.The wound should be covered with light
dressing. Please keep the wound site clean and avoid making the dressing wet
during shower. Always change dressing if wet.You may need to come back to the clinic for
suture removal 1 week after the procedure if any. You may remove the dressing
2-3 days after suture removal.Please avoid lifting the affected arm for 1
month and avoid vigorous arm movement in the first week after the procedure.You will be arranged to attend regular ICD
analysis, re-programming and battery power assessment.Please carry your ICD identity card at all
times.Follow your doctor’s instructions or refer
to the information booklet from the ICD company to minimize the risk of
pacemaker malfunction due to electromagnetic interference. In general, strong
electro-magnetic field or radiofrequency signal will interfere your ICD. Please
keep a distance of >15 cm (6 inches) from an active mobile phone. Household
electrical or electronic appliance usually does not affect ICD.You should report to your doctor or nearby
Accident and Emergency Department if you suffer from syncope or electric shocks
delivered by the ICD.ICD generator will need to be replaced in
3-6 years’ time when the battery is depleted.
AfterProcedure:
You may be discharged from hospital several
days after the CRT implantation.The wound should be covered with light
dressing. Please keep the wound site clean and avoid making the dressing wet
during shower. Always change dressing if wet.You may need to come back to the ward or
clinic for suture removal 1 week after the procedure if any. You may remove the
dressing 2-3 days after suture removal.Please avoid lifting the affected arm for 1
month and avoid vigorous arm movement in the first week after the procedure.You will be arranged to attend regular CRT
analysis, re-programming and battery power assessment. To maximize the benefits
of CRT, the settings will be optimized with the help of echocardiogram.Please carry your CRT identity card at all
times.Follow your doctor’s instructions or refer
to the information booklet from the CRT Company to minimize the risk of CRT
malfunction due to electromagnetic interference. In general, strong
electro-magnetic field or radiofrequency signal will interfere your pacemaker. Please
keep a distance of >15cm(6 inches) from an active mobile phone. Household
electrical or electronic appliance usually does not affect pacemaker.CRT generator will need to be replaced in
5-10 years’ time when the battery is depleted.
Atrial Septal Defect Occluded
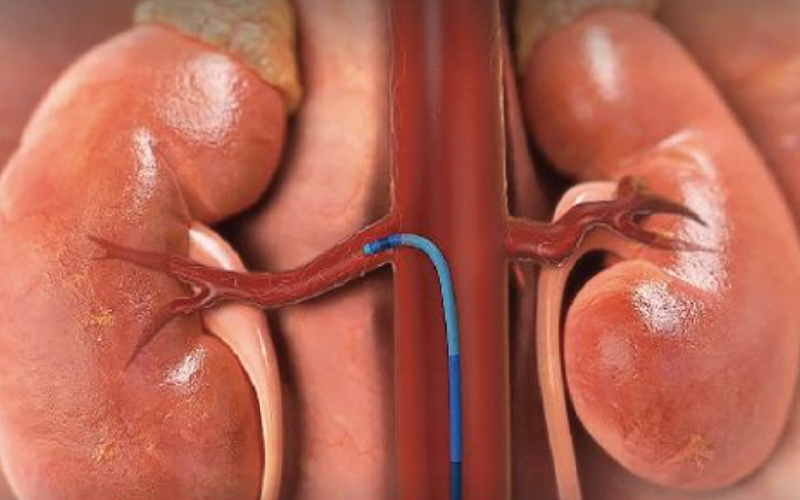
Renal Denervation System (RDN)
透過腎臟交感神經消融術,將過度活躍的交感神經切斷,減低荷爾蒙腎素的分必量,從而降低血壓水平,保障病人心臟,腎臟及血管健康。按此了解更多腎臟交感神經消融術按此了解更多手術推廣優惠併發症:血壓波動心跳停止死亡使用顯影劑引起的後遺症心律受干擾(例如心跳過慢)血液凝塊血管受損而需手術治療使用止痛或抗焦慮藥物引起的後遺症過程:這項手術會在心導管檢查及介入治療室內進行,通常只需局部麻醉。手術需時約45至60分鐘。護士會在你的胸口貼上電極以便監察心率及心跳,並為你戴上血氧量監察器。血壓量度器亦會不時從你的手臂量度血壓。醫生會穿刺大腿內側(腹股溝),以便進入動脈,然後在X光引導下將不同導管送入腎臟血管。當導管被順利置入其中一邊的腎臟動脈後,醫生會開始將(射頻能量) 經導管傳送至腎臟動脈壁上數個適合治療的位置,每個位置需時1分鐘。病人可能會感到下腹有些微熱脹,但維持時間短。當一側腎動脈成功接受治療後,醫生會在另一側腎動脈重複以上步驟。整個手術完成後,醫生就會從病人體內取出所有治療導管器材。術後跟進:一般情況,病人可在手術翌日出院。出院前,醫護人員會檢查傷口,並蓋上消毒紗布。請保持傷口清潔,如消毒紗布被弄濕,請立即更換。一般情況下手術後第2天可淋浴。為防止傷口流血,在最初7天內應避免進行劇烈運動。傷口附近的瘀傷大多是輕微的,通常會在手術後2至3星期消失。如發現傷口滲血/液、腫脹或發炎等問題,請立即返回醫院求醫,或到附近急症室就診。術後護理及持續管理高血壓:接受高血壓導管治療(RDN)療程後,病人仍需努力維持良好健康的生活習慣,嚴格遵守醫生指示,保障健康及防止血壓再度失控:1. 立即戒煙吸煙會加速心跳頻律及令血壓上升,增加心臟病發及中風的風險。如您想決心戒煙,請向醫生查詢戒煙方法。2. 避免飲酒若有飲酒過量習慣,會令血壓長期增高。3. 增加運動量定期運動有助降低血壓及膽固醇,協助維持理想體重,亦有助減低日常生活中的壓力。4. 選擇健康飲食健康飲食的原則是少攝取飽和脂肪丶膽固醇及鈉,多吃含豐富蛋白質的食物,以及新鮮水果、蔬菜與小麥製食物等,有助維持理想體重,控制血壓及膽固醇。5. 妥善管理壓力壓力似乎是現代都市生活中難以避免的「副產物」,但我們可學習以各類減壓方式,從而將壓力對身體健康的無形破壞減低。研究發現,減壓技巧有助我們的抗壓能力,從而調節我們的各種因壓力而起的生理反應,包括心跳加速、血壓上升及荷爾蒙分泌異常等。6. 繼續準時服藥若醫生已就你的高血壓病情處方藥物,請緊記遵照指示,定時定量服用,讓藥物發揮功效。請勿在未經醫生許可下,自行停藥或更改服藥劑量,否則血壓可能再次回升。如對藥物副作用感到困擾,請通知醫生。現時抗高血壓的藥物種類繁多,醫生可根據病人需要,處方最適合的類別。常見問題:1. 手術會否影響腎臟正常功能?答:臨床測試發現,接受RDN療程後,病人的腎臟功能正常,亦無出現與腎臟相關的併發症。在成功的腎臟移植個案中,亦證明了這些腎臟神經線被消融與否,同樣不影響腎臟正常功能。2. 手術後,患者是否無需再服藥?答:手術後數個月內,療程會逐漸發揮降低血壓的功效,病人需要繼續按醫生指示服用藥物,血壓會得到較佳控制,請勿自行停藥或轉藥。